In the world of medical advancements, gene therapy stands out as one of the most promising and revolutionary innovations. As a field of biotechnology, gene therapy holds the potential to treat, and in some cases, cure previously untreatable genetic diseases by directly altering the genetic material of a person’s cells. This process, which involves either replacing, inactivating, or introducing genes into a patient’s cells, could offer new hope to millions of people suffering from a wide range of genetic conditions, such as cystic fibrosis, hemophilia, sickle cell anemia, and muscular dystrophy.
The journey from concept to reality in gene therapy has been long and complex, with successes and failures, but recent breakthroughs have brought us to the cusp of a new era in medicine. This article will explore the mechanisms of gene therapy, its current and potential applications, ethical considerations, challenges, and the future of biotechnology in transforming human health.
1. What is Gene Therapy?
Gene therapy is a medical treatment that involves modifying the genes inside a person’s cells to treat or prevent disease. Essentially, it seeks to correct genetic mutations at the source—by altering the DNA sequence in the cells that are responsible for causing a particular disease. In this approach, the goal is to directly address the underlying cause of genetic disorders rather than merely alleviating symptoms.
Gene therapy can be performed in two primary ways:
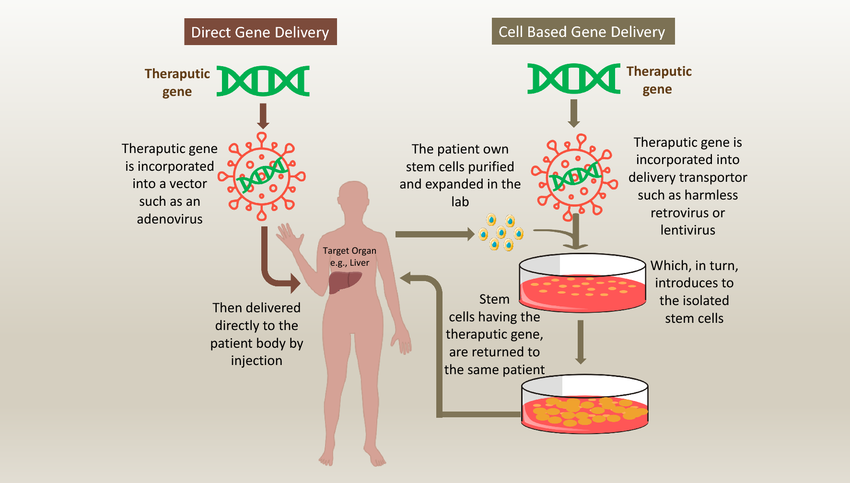
a. In vivo Gene Therapy
In in vivo gene therapy, therapeutic genes are delivered directly into the patient’s body. The genes are typically delivered using a viral vector (such as an adenovirus or lentivirus), which carries the genetic material into the target cells. Once inside, the new genes are incorporated into the patient’s DNA, ideally correcting the mutation or providing a new function to the cell. This method is often used for diseases affecting specific organs, such as the liver or lungs.
b. Ex vivo Gene Therapy
In ex vivo gene therapy, cells are removed from the patient’s body, modified in the laboratory, and then returned to the patient. For example, a patient’s bone marrow cells could be extracted, genetically modified to correct a defect, and then transplanted back into the patient. This method is often used in the treatment of blood-related disorders, such as sickle cell anemia and certain types of cancer.
Both methods are designed to target the root cause of genetic diseases by repairing or replacing faulty genes, potentially offering long-term or even permanent solutions to conditions that previously had no cure.
2. How Gene Therapy Works: The Science Behind the Treatment
Gene therapy works by introducing, altering, or removing genetic material within a person’s cells to achieve therapeutic benefits. The most common approaches to gene therapy include:
a. Replacing a Mutated Gene
In many genetic diseases, a mutation in a gene causes the body to either produce a defective protein or fail to produce a necessary protein at all. By replacing the mutated gene with a functional copy, gene therapy aims to restore normal function. For example, cystic fibrosis, caused by mutations in the CFTR gene, can be treated by introducing a healthy version of the gene to restore proper function of the protein that regulates mucus production in the lungs.
b. Inactivating or “Knocking Out” a Mutated Gene
Sometimes, diseases are caused by a gene producing a protein that is toxic or harmful to the body. In these cases, gene therapy can work by silencing or “knocking out” the defective gene. For example, in Huntington’s disease, a mutation in the HTT gene leads to the production of a harmful protein. Gene therapy can aim to stop the expression of this gene to reduce the damage caused by the mutant protein.
c. Introducing a New Gene
Gene therapy can also introduce entirely new genetic material into a patient’s cells to enable them to produce proteins that are missing or insufficient. For example, in hemophilia, patients lack the clotting factor protein due to genetic mutations. By inserting the correct gene that codes for this protein, gene therapy can enable patients to produce the protein naturally and avoid dangerous bleeding episodes.
The development of viral vectors, nanoparticles, and other delivery mechanisms has been essential in improving the effectiveness of gene therapy. Since genes are too large to be delivered directly into the cell by other means, these delivery systems are crucial to the success of gene therapy.
3. Applications of Gene Therapy: A New Era of Medical Treatments
Gene therapy has already demonstrated significant promise in treating several genetic disorders, and it is likely to expand into many other areas of medicine in the coming decades.
a. Genetic Diseases
Many genetic diseases that were once considered untreatable may now have viable therapeutic options through gene therapy. Some of the most well-known applications include:
- Cystic Fibrosis: By introducing a healthy copy of the CFTR gene, gene therapy has shown potential in restoring the function of the lungs in cystic fibrosis patients, reducing symptoms and improving quality of life.
- Sickle Cell Anemia: Gene therapy is offering hope for people with sickle cell anemia by introducing a functional copy of the hemoglobin gene or by editing the sickle-cell-causing mutation in patients’ blood cells. Early clinical trials have shown promising results in eliminating the need for blood transfusions and reducing symptoms.
- Hemophilia: Hemophilia, a bleeding disorder caused by defective clotting factors, is being treated by delivering a functional version of the Factor VIII or Factor IX This gene therapy could significantly reduce the need for frequent blood infusions and improve life expectancy.
b. Cancer Therapy
Gene therapy also has potential in oncology. Cancer cells often contain mutations that allow them to proliferate uncontrollably. Gene therapy can be used to modify the genetic makeup of cancer cells or even enhance the immune system to recognize and attack cancer. CAR T-cell therapy, a form of gene therapy, involves modifying a patient’s T cells to better recognize and attack cancer cells. This method has already shown promising results in treating certain blood cancers, such as leukemia and lymphoma.
c. HIV Treatment
Gene therapy could also hold the key to managing and possibly curing HIV. Recent research is focused on modifying patients’ immune cells to make them resistant to HIV infection. This approach could either involve editing the CCR5 gene, which HIV uses to enter cells, or enhancing the immune system’s ability to recognize and eliminate the virus.
d. Age-related Diseases
Although still in the early stages, gene therapy could eventually be used to treat age-related diseases, such as Alzheimer’s and Parkinson’s. By repairing or replacing damaged genes associated with these neurodegenerative diseases, gene therapy may offer new avenues for slowing down or reversing the progression of these conditions.
4. Challenges and Ethical Considerations in Gene Therapy
While gene therapy represents a groundbreaking advancement in biotechnology, several challenges and ethical issues must be addressed before it can become a routine treatment option.
a. Safety and Efficacy
One of the major hurdles in gene therapy is ensuring that the therapy is both safe and effective. Early trials have faced challenges with immune reactions, insertional mutagenesis (when the inserted gene causes unintended changes in other genes), and limited duration of gene expression. Ensuring long-term safety without adverse effects is essential for the widespread use of gene therapy.
b. Accessibility and Cost
Gene therapy can be incredibly expensive, often costing hundreds of thousands of dollars per patient. The cost of gene therapy treatments may be prohibitively expensive for many people, especially in low-income countries or among those without comprehensive health insurance. As with any advanced medical technology, equitable access to gene therapies will be a critical issue moving forward.
c. Germline Editing and Ethical Boundaries
While gene therapy often focuses on treating individual patients, advances in biotechnology have also led to discussions about editing the human germline—the DNA that can be passed down to future generations. CRISPR-Cas9 technology, which allows for precise gene editing, has raised concerns about designer babies, genetic enhancement, and the possibility of unintended consequences. The ethical implications of germline editing are still being debated, with many experts calling for strict regulation and oversight.
d. Informed Consent
As gene therapy continues to evolve, patients must be fully informed about the potential risks, benefits, and unknowns associated with these treatments. Ethical guidelines regarding informed consent will be essential to ensure patients understand the implications of altering their genetic material.
5. The Future of Gene Therapy: A Transformative Medical Revolution
The future of gene therapy looks incredibly promising. As technology advances, more diseases will be treatable, and the safety and effectiveness of therapies will continue to improve. Ongoing developments in genetic editing tools, nanotechnology, and delivery systems are poised to make gene therapy more accessible, precise, and scalable. Additionally, the increasing availability of genetic sequencing will help doctors diagnose diseases earlier, allowing for the identification of genetic conditions that could benefit from gene therapy.
With advancements in personalized medicine, gene therapy could become a part of routine treatment regimens, not just for rare diseases but for more common conditions as well. The ability to edit genes with precision could unlock cures for genetic disorders, extend human lifespan, and transform how we approach healthcare.
6. Conclusion
Gene therapy, fueled by the power of biotechnology, is transforming human health in ways once thought impossible. From curing genetic disorders to advancing cancer treatment, the possibilities are immense. However, as with any groundbreaking technology, there are challenges to overcome—scientific, ethical, and financial. As we move forward, continued innovation, ethical discourse,